https://commons.wikimedia.org/wiki/File:Hamstring_tear_(48605452627).png, Injurymap, CC BY 2.0 <https://creativecommons.org/licenses/by/2.0>, via Wikimedia Commons
Deborah Tosline wrote and published “Skin Remodeling DIY: An Introduction to the Underground World of Do-It-Yourself Skincare” in 2015. Her approach to skin care is based on a scientific background, love of research and over 40 years of DIY skincare experience.
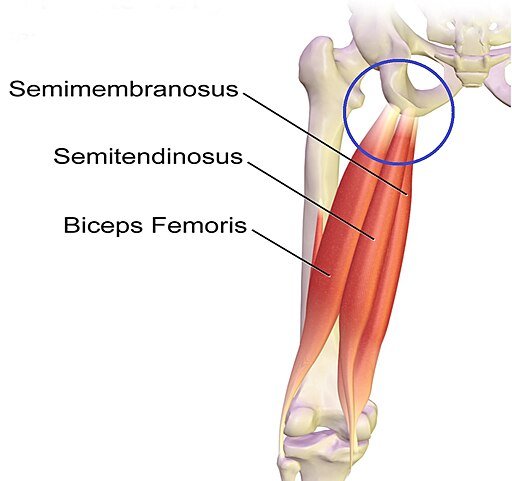
Hamstring injuries are one of the most common sports injuries, however a complete Proximal Hamstring Avulsion (PHA), where the hamstring tendons tear away from the bone, is a rare injury. I recently sustained a full PHA, chose surgical repair and am now on the slow recovery path. In my experience, there is little information available about recovery from PHA surgery. I write about my experience hoping that this information will help others. Not surprisingly, PHA recovery involves the same biochemical healing cascade and collagen development phases for soft tissue repair as for advanced skin care.
While I searched for information regarding PHA surgery recovery, I found a YouTube post that led me to a private Facebook group. To learn about other PHA recovery experiences check out:
https://commons.wikimedia.org/wiki/File:Opgespannen_hamstrings_(cropped).jpg, Paul Hermans, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
A PHA typically results from a sports injury due to an explosive movement such as sprinting or jumping or a fall. The tendon is susceptible to tearing when the hamstring is lengthened during an eccentric contraction that occurs when the hip is flexed at the same time that the knee is extended. A proximal hamstring rupture may result in loss of function, discomfort while sitting, poor outcomes and disability if undiagnosed or misdiagnosed.
Risk factors for a PHA include:
shortened muscle length,
lack of flexibility,
insufficient warm-up,
lower back injury,
and tight muscles and fascia that impede nerves from gliding freely.
Over the past 36 years I’ve walked four miles, hiked or done other cardio an hour a day for four to six days a week and have practiced yoga one to four days a week for about 32 years.
https://commons.wikimedia.org/wiki/File:Hamstrings-animation.gif, Niwadare, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Despite my efforts to stay strong and flexible, my PHA injury left me mostly bedridden for a couple of months. Prior to my injury I had an uncomfortable tightness in my right hamstring and hip and although I consistently attempted to loosen and strengthen these muscles, I did not go to a doctor or physical therapist (PT). I’ve never hired a personal trainer.
On Saturday, February 3rd, I tried pickle ball for the first time. Although I’ve played racquetball and tennis, I had not played a court sport for years. Before playing, I did not warm up. I wore Vibram-sole bare-foot shoes instead of court shoes. The game began. At one point, I dove for a ball and felt 3 pops at my sit bone. I was taken aback, I knew that something had happened but I did not feel pain. I did not know what to do. I stayed on the court, reached for another ball and felt three more pops. I still did not feel pain but I experienced intense nausea, felt a huge loss of strength and stability and I left the court.
For reasons that I will not get into here, I don’t feel physical pain in the same way that others may experience pain. I have pain but my brain processes it differently, it may be delayed or take a different form. I may not feel or interpret my injuries and may not tell anyone. I rarely go to the doctor for physical injuries.
Internal bleeding from PHA, photo of and by author, 2/8/2024.
Immediately after the injury, my upper leg and hip muscles became locked and hard. I began researching my symptoms and realized that I had torn my hamstring tendon but I did not know if it was a partial or complete tear. I barely got out of bed for four days. I could not sit on my injured leg and was terribly nauseous. These symptoms showed me that I was in a great deal of pain. A PHA may result in internal bleeding and I had a hematoma that traveled down the back of my leg towards my knee due to gravity. I finally shared my injury news and was prompted to go to a doctor.
A PHA tear may remove bone. An osteopathic emergency room x-ray showed that my bone was intact. An MRI was ordered. I saw an osteopathic surgeon who informed me that my MRI showed a complete PHA and that my hamstring tendons had retracted 2.5 centimeters away from the bone. Surgery was recommended and non-surgical treatment referred to as “conservative treatment” was also offered as an option. Both treatments require long recovery protocols and PT. I chose to have the surgery as soon as possible to avoid further hamstring retraction and to ensure that my hamstring tendons reattach at the bone instead of my sciatic nerve or other nearby soft tissue.
After surgery was scheduled. I prepared myself to be on crutches for six weeks. I would be unable to bend down and pick items up from the floor and have limited ability to complete daily self-care activities.
Recovery needs are personal and different for everyone. I made the following preparations:
Made healthy home-made whole food snacks, portioned and froze.
Made organic vegan meal delivery arrangements for two weeks.
Purchased two grabbers and a “hip surgery” package with two more grabbers and other tools.
Secured a three-shelf rolling metal tray.
Ensured six weeks of dry goods and household items.
Purchased a high rise toilet seat
Found two rubber water bottles that I filled with rubbing alcohol and water and used as ice packs.
Established a temporary red and near infrared light station.
Gathered pillows to elevate my surgery leg.
Compiled boy short undergarments and suitable comfortable clothing.
Ensured that electronics and charging stations were accessible.
Placed standard personal care and household items at waist height.
Temporary photobiomodulation station with near-infrared lights. Photo by author, 2/19/2024.
While waiting for PHA surgery, I continued to recover from my PHA injury. The initial swelling went down within the first week. I was not able to sit on my injured side and leaned on my uninjured leg while briefly sitting. I lounged. I used my PBM station. About one and one-half weeks after my injury I began to slowly move around the house. My unattached hamstring felt more stable each day. As I felt stronger, I slowly began walking about 2 miles a day prior to surgery to maintain muscle mass.
As I recovered from the injury I felt good and wondered whether I should proceed with surgery. Then I remembered the detached muscles that I’ve seen that had slid away from the bone, I did not want that for my hamstring. I accepted that I would start my recovery all over again and that it would now include a deep surgical incision and bone trauma. The associated fascia and nervous system disruption are uncomfortable.
On February 27, 2024 I had open incision PHA outpatient surgery. The anesthesiologist used a spinal block prior to surgery to minimize post-surgery swelling and inflammation. A four-inch incision was made horizontal to my thigh at the crease between the buttocks and thigh. Three dissolvable screws were placed in the bone and the hamstring tendons were sutured to the screws.
Osteopathic surgeons prescribe varying recovery protocols for PHA post-operative (PO) surgery and PHA patients have different experiences with pain, ability and recovery. I describe my surgeon’s recovery protocols, the methods that I use to support my recovery and my personal experience in the following text.
Waterproof bandage. Photo by and of author, 3/1/2024.
My surgeon’s PHA surgery recovery protocol included:
A waterproof bandage placed over a glue bandage, placed over the incision.
Crutches for six weeks.
Non-weight bearing on surgery leg for two weeks.
25 percent (%) toe-touch weight bearing third week.
50% toe-touch weight bearing fourth week.
75% toe-touch weight bearing fifth week.
100% toe-touch weight bearing sixth week.
Do not sit on incision for 6 weeks.
Remove waterproof bandage 7 days after surgery.
Remove glue bandage two weeks after surgery during doctor follow-up visit.
May drive after six weeks.
Begin PT after six weeks.
Wear a hip/leg brace for six to eight weeks.
After surgery, I felt unstable but overall, pretty good. I had minimal inflammation. I managed pain and discomfort using:
Rick Simpson Oil (RSO) with or without delta 9 THC every two hours for pain relief and inflammation after surgery for about 7 days.
First night, one pain med at 12:30 a.m. when I could not fall asleep and wondered if I had pain that was not registering in my brain.
Ibuprofen twice a day for two days, once a day for two days, I don’t remember why, I think it was to get ahead of potential inflammation. I don’t usually use.
Surgery leg elevated constantly – even as I write this.
Ice for 20 minutes every two hours first 5 days; after the first week I switched to using ice once at night before I sleep.
After about ten days I began using daily photobiomodulation (PBD) with red and near infrared lights and later green light therapy for pain, inflammation and healing.
Castor oil – I used cold-pressed organic castor oil externally for inflammation and soft-tissue health
Author photo, 3/20/2024.
As I publish this article, I am 33 days PO and have six months to a year for a full recovery and return to previous activities. My personal observations during my recovery:
I am grateful and thankful for my daughter, neighbor and friends who’ve helped me during my recovery. Your support helped me so much with my recovery. Love to you all.
First week - I felt unstable, uncomfortable, and exhausted. I used the leg lifter in the hip package to lift my leg into and out of bed for a few days, I was glad to have it. I began a daily set of ankle rolls in both directions and ankle pumps to enhance circulation in my surgery leg while immobile. As feeling returns there are a variety of sensations in the vicinity of the incision and hamstring. The sensations continue throughout recovery and range from pain to electrical sensations to odd zingers.
Second week - I developed a stomach issue which set me back nutritionally. I was still uncomfortable and exhausted. I began standing in front of my PBM station for 10 minutes a day to reduce pain and inflammation and to enhance healing.
Third week - I was able to do more self-care and some home maintenance although I tired easily and still felt unstable. Took my first shower, I had been using body wipes and “sponge baths.” I felt a bit insecure, but the shower was great. I stood in front of the PBM lights for 20 minutes a day.
Fourth week - I moved to a new day-time lounging location with my PBM station. The lounging allows me to increase my red and NIR light usage and apply the light treatment to different areas. I finally was able to view and photograph my incision to inspect it. After five days of increased PBM usage, my incision healed dramatically, you’ll have to take my word.
Fifth week – I began applying 75% TTWB on my surgery leg. I had less discomfort at the incision and I began to feel more stable. As I lounge, I feel as if I am leaning on something hard at my incision site. This is the PHA surgery “sitting on a baseball” feeling. I hope that this will go away over time as the screws dissolve and I begin PT and fascia/scar tissue massage. I’ll understand the extent of this feeling more when I can begin to sit next week. I slowly crutched about 2,000 steps a day and around the block several times this week to test my ability and to prepare to walk again.
Sixth week – starts on 4/2. I will begin using 100% TTWB and will only use the crutches for stability. I am excited see what it feels like to put all of my weight on my surgery leg as I prepare to walk in another week. I continue to wear the hip/leg brace and may have to wear it for eight weeks.
I may have been able to prevent this injury if I had made the following choices over time:
went to the doctor to evaluate osteopathic and muscular conditions.
worked with a trainer to ensure holistic balanced muscular strength and flexibility.
worked with a physical therapist for conventional care of all injuries and recoveries.
researched and physically prepared to play a new sport.
warmed-up before explosive, dynamic movements.
Author at 65, photo 3/20/2024.
Overall, I have an optimistic recovery perspective. This is a tough injury. The biomechanics of the hamstring tendon to bone connection can never be replicated. Scar tissue is not specialized, a bit stiff and will not substitute for the intelligence of the original tendon to bone mechanics. As a result, there is a potential to retear the repaired hamstring tendon.
My goal is to diligently follow PT recovery protocols to promote full function. In addition, I’ve learned that in the future it is important for me to utilize professionals who are gratefully available to me to ensure that I have balanced strength and flexibility as I age to prevent injuries. I will continue to integrate allopathic and naturopathic healing modalities to optimize prevention and treatment of health issues.
If you need more information remember to check out:
It would be an honor to me if you purchased my facial care book. Thank you!
Take good care of yourselves!
XO Deborah
This article is intended to be used as general information only and is in no way intended to replace medical advice, be used as a medical treatment program, diagnosis, or cure of any disease or medical condition. There are no warranties, expressed or implied, regarding the effectiveness of the practices described in this article. Products or substances discussed herein are for educational purposes only and are not intended as recommendations of the author.